Influenza: cause or excuse? An analysis of flu’s influence on worsening mortality trends in England and Wales, 2010–19
Lu Hiam, Martin McKee, and Danny Dorling, writing in the British Medical Bulletin, 15 January 2024, All social groups in England and Wales experienced a long period of increasing life expectancy until the second decade of the 21st century, a trend mirrored within Scotland and Northern Ireland, albeit not as favourably in recent decades. Life expectancy, the most widely used summary measure of a population’s mortality experience, shocked observers when its long upward trend slowed markedly shortly after 2010. Recent gains even reversed in some groups, such as those living in poorer areas. This slowdown was also witnessed throughout the rest of the UK. Although we focus on England and Wales, some other European countries also saw slowing life expectancy improvements. However, the situation in the UK was more severe and prolonged than elsewhere in Europe, similar to what was observed in the United States. For comparison, between 2010 and 2021, life expectancy at birth increased by 0.5 and 0.3 years for women and men respectively. In contrast, the corresponding figures in Sweden were 1.4 and 1.6 years; in France, they were 0.8 and 1.4 years; and in Germany, one of the poorest performers in continental Europe, they were 0.6 and 0.7 years.
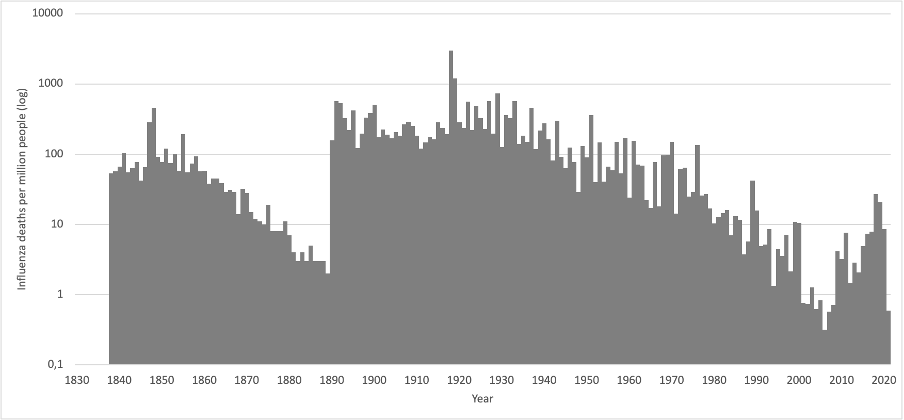
Life expectancy tends to fluctuate yearly, especially in countries with small populations where the impact of relatively few deaths can be significant. In contrast, a non-trivial change in a large country like the UK usually has an identifiable cause. For instance, life expectancy in England and Wales fell by 0.45 years between 1950 and 1951 and 0.37 years between 1967 and 1968. These decreases coincided with what was considered an influenza epidemic and a confirmed influenza pandemic, respectively.9 While there is ongoing debate about the exact causes of the high death toll in 1950/51, which was much higher than in other countries, the impact of the 1968 influenza pandemic is uncontested. The underlying upward trend in life expectancy has been attributed to reduced risk factors, especially for smoking-related cancers and cardiovascular diseases. This decrease in risk reflects improved living conditions and, particularly since the 1960s, advancements in the effectiveness and coverage of healthcare. While there is some debate about the detailed explanation of these improvements, health overall in the UK was improving. There was a widespread, albeit implicit, assumption that this would continue. However, something changed in 2012. Unlike the previous years mentioned, this was not a one-off decline but a shift in the longer-term trend.
…
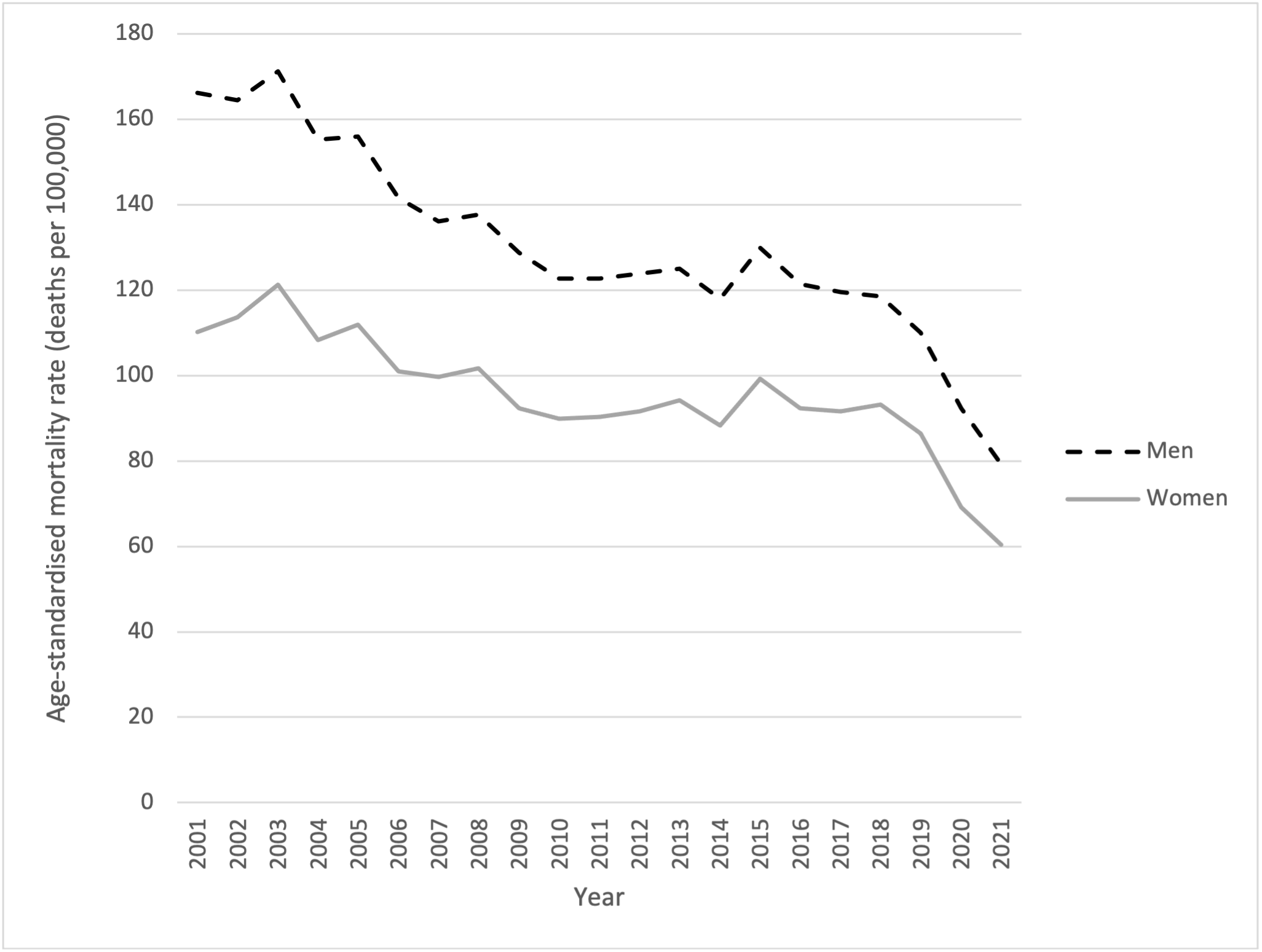
Figure 5: Age-standardised mortality rate, deaths per 100,000 population, for influenza-like disease, males and females in England and Wales 2001 to 2021. Note: deaths due to the spread of Sar-CoV2 are not included.
…
Influenza did not cause the stalling and worsening mortality trends in England and Wales from 2012 onwards, which continue to the present day. Given the evidence of the greatest impact of austerity on those living in deprived areas, a next step will be to examine these trends by deprivation decile. Future research may also explore why so many people in such high positions of authority were so quick to attribute the change in overall mortality trends to influenza and were slow to correct this later and why, to this day, the negative impacts of austerity on health, not least on pandemic preparedness, are not accepted by its architects, nor by so many of those who have followed them; and why so many people in England and Wales have stood by and watched this failure of government and public health unfold.
For the full British Medical Bulletin paper and supplementary material click here.