Declining health outcomes, rising health inequality and extreme economic inequality
Evidence is beginning to surface of the possible health effects of the rapid social polarisation that is taking place in the UK. This evidence is often hidden, or at the very least hard to find, but it will soon emerge more fully into public debate. In September 2015, at the annual British Sociological Association Medical Sociology conference at the University of York, I used the following graph to show that there has been a stalling in one of the key official indicators of health improvement in the UK in recent years. The indicator concerns Potential Years Lost of Life or early mortality, among men (see Chart 1).
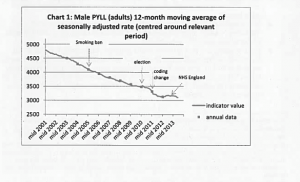
Chart 1: Source: http://www.lgcplus.com/Journals/2015/05/22/e/i/u/QCRC-Board-Paper—copy-version-2.pdf “Quality and Clinical Risk Committee Paper – NHS England – October 2014
The document, that this graph came from, was found in a report prepared as background material for a meeting that was held a year ago titled: “Medical Directorate Senior Management Team Meeting, 2 October 2014, 4d Deterioration in Rate of PYLL Improvement”. The document is marked “In confidence – not for publication” – but it is on an open access website – anyone can read it and it has been on the website for many months. Unless it is soon removed anyone can find a copy (other interesting background information is available here).
Within the medical directorate’s document of October 2014 was the following statement: “The attached analysis, which is based on new provisional mortality data that we have obtained from ONS shows that PYLL in men has been improving steadily until 2010, but in 2012, 2013 and 2014 the improvement has been much more gradual. Further, male PYLL is likely to have deteriorated for the first time in 2013 and this deterioration is partly linked to a particular peak in male PYLL in April 2013, which is as yet uninvestigated.”
Clearly there are considerations as to whether the introduction of the tenth International Classification of Disease (ICD10) coding changes may have influenced the trend. That is what the word “coding” on the graph refers to. However, there are also political considerations, as the addition of the word “election” on the original graph made clear. What we know is that the long-term improvements in years of life lost due to premature mortality is beginning to stall; although we only know it if we are good at using Google and understand acronyms well.
For NHS England and Public Health England PYLL is a key statistical indicator: Potential Years of Life Lost (PYLL) is a measure of premature deaths attributable from causes considered amenable to healthcare. It is the NHS Top Indicator, Labelled 1a, and is the primary key outcome measure that NHS England asks Clinical Commissioning Groups (CCGs) to monitor. The earlier someone dies as a result of a cause of death that is treatable or otherwise preventable, the more that damages this measure. For the years 2013/14, PYLL was described as the “Overarching indicator” to be used to monitor health in England. Given that, it is odd that as yet concerns about recent trends in health outcomes in the UK have been so muted.
For a year it has been known that improvement in the PYLL indicator is stalling for men. For longer we have known that female life expectancy in old age has been declining in the UK since shortly after that 2010 election. In April 2015 it was suggested that the sudden drops in female life expectancy in the UK could be due to the rise in smoking among women in the past. However, that rise in smoking among women was not a sudden affair, and even if it had been the impact decades later would have been spread over several years, it would not have been so sudden. For both men and women in the UK past improvements in health outcomes are either rapidly stalling or actually reversing.